Could psychedelics help us manage post-pandemic PTSD?
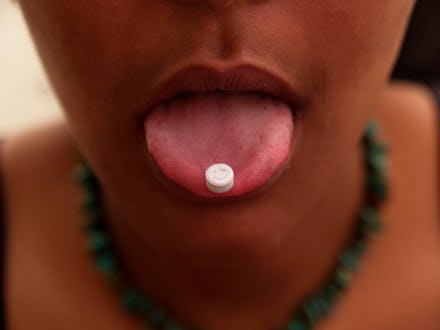
Psychedelics like psilocybin (the main compound in magic mushrooms), LSD, and MDMA have been experiencing a renaissance during the last few years. Recent studies have highlighted their promise in treating a number of mental illnesses, including post-traumatic stress disorder, or PTSD. Despite this renewed interest, though, the illegality of these substances and the general stigma surrounding them makes conducting the research required to validate their therapeutic potential a long, uphill process. At the same time, the pandemic and ensuing existential crises may leave a number of us with PTSD, once again raising questions about the need to accelerate psychedelics research.
“This is huge, and we’re nowhere near being out of it,” says Charles Grob, a professor of psychiatry and behavioral sciences and pediatrics at the David Geffen School of Medicine at UCLA, whose research focuses on psychedelics, of the pandemic. “It’s going to have a very significant impact on the general population for all sorts of reasons,” such as a lack of social connection, as well as loss, whether of loved ones, employment, or a sense of normalcy. Stay-at-home orders might confine people with abusers, and there have been reports of a rise in domestic violence. “I think people are vulnerable to being traumatized during a long, sustained pandemic.”
It's important to note that, thankfully, the majority of us probably won’t develop PTSD, a disorder that develops in the wake of a traumatic event, with symptoms such as nightmares, flashbacks, and avoidance of reminders of the trauma. The few who do would include those who were seriously ill with COVID-19, the frontline healthcare workers caring for them, and those who’ve lost loved ones to the disease, says Petros Levounis, professor and chair of the department of psychiatry at Rutgers New Jersey Medical School. Based on studies of 9/11 and other tragedies, out of those highly exposed to the traumatic effects of COVID-19, “maybe a third will develop PTSD.” The rest would likely experience lingering, but less severe, psychological effects, such as hyperarousal, discomfort, and malaise, from which they would eventually recover.
But even if most of us won’t emerge from the pandemic with full-on PTSD, those who do would still comprise “a small but significant proportion,” Grob says. Compared to, say, a wartime scenario, which would lead to a much higher incidence, “here the trauma is more of a quiet trauma of isolation and perhaps feelings of hopelessness and helplessness. It’s more of an existential crisis,” he explains. “There’s a collective sense of vulnerability to this virus.” People can lose purpose and meaning, impairing their ability to function and eroding their sense of self.
Should those who develop pandemic-related PTSD seek the treatments currently in use, they would take medications, including selective serotonin reuptake inhibitors (SSRIs, such as Zoloft and Paxil) and benzodiazepines (like Xanax); and/or exposure therapy, a broad category of therapy that, true to its name, requires revisiting the trauma with a therapist, says Matthew Johnson, a professor of psychiatry and behavioral sciences at Johns Hopkins Medicine.
Psychotherapy has yielded pretty good results, according to Grob, but “there’s always room for improvement.” Johnson is more critical. “We drastically need better treatment options,” he says. “Exposure-based psychotherapy works really, really well if people complete it. The problem is, adherence is extremely low.” Understandably, few people are willing to attend weeks of therapy sessions digging deep into their trauma. Medications help, but not much. Johnson doesn’t discourage trying them — anything that helps a little is worth taking — but says they mainly mask symptoms without tackling the underlying cause and can worsen existing problems, like addiction.
Although they’re medications, psychedelics are more similar to psychotherapy in how they work, Johnson explains. When used correctly, they basically allow people to reap the benefits of therapy very quickly, rather than in weekly meetings over the course of a month. In one clinical trial, 68% of the veterans, firefighters, and police officers studied no longer met the criteria for a PTSD diagnosis after just two MDMA-assisted psychotherapy sessions.
When people with PTSD take psychedelics, “they reprocess their trauma,” says Johnson, who’s studied these substances since 2004. They emerge with a story about how they, and their thinking about their trauma, have changed. “The pharmacological effect is one of inducing mental flexibility and broadening perspective taking. That’s the stuff that allows psychotherapy to unfold.” The idea is that people would take these substances under the supervision of a therapist, who would help them set an intention for the psychedelic experience, process any material that arises during it, and place the experience in the context of their intention in later sessions, Grob explains.
The findings on MDMA have been particularly encouraging. A number of clinical trials of the drug are moving into phase 3 trials, the final phase before FDA approval, Johnson says. “That work is very promising. That shows a very large effect on PTSD.” Grob agrees. He points to recent phase 2 trials led by Michael Mithoefer of the MAPS Public Benefit Corporation as especially promising, including the one on first responders and military vets described above.
There haven’t been any clinical trials yet of so-called classic psychedelics, like psilocybin, LSD, and mescaline, for PTSD, Johnson says. But he’s secured funding for the first, on the use of psilocybin for PTSD, planned to start within the year.
The hurdles to such research loom large, he tells Mic. Obtaining approval to work with Schedule I controlled substances — drugs the Drug Enforcement Administration has deemed to have zero medical value and a high potential for abuse— “takes a lot of time and money.” But an even bigger hurdle is the lack of funding from the National Institutes of Health, possibly because of perceptions of psychedelics research as “too risky,” as well as its associations with counterculture woo-ness. “If you called this anything else and described the results [so far], this would be getting hundreds of millions of dollars of funding,” Johnson says.
While he supports such research efforts, Levounis doesn’t believe the link between the pandemic and PTSD is strong enough to warrant expanding them. He sees a lack of access to existing therapies as a greater priority. “What we have is effective, but we have not been able to find those who need it most all that easily.” He also points out that most of the research on psychedelic-based treatments for PTSD focus on severe forms of the disorder, which, again, most of us won’t experience.
Grob worries about rushing out large-scale psychedelic-based PTSD treatments à la Operation Warp Speed (the Trump administration’s partnership with manufacturers to produce COVID-19 vaccines and distribution materials ahead of the vaccines being FDA-approved), which could increase the risk of problematic reactions. “We don’t need an Operation Warp Speed,” he says. “We’ve got some really good findings from the Mithoefer studies. Those findings need to be carefully built upon.” And while psychedelics research requires jumping through regulatory hoops, he says his group has shown it’s possible.
Johnson has a similarly cautious view. “I’m about smart tweaks to move things along” — that is, those that allow the research to remain evidence-based, he says, but believes re-scheduling psychedelics and NIH funding would provide a helpful nudge. He thinks COVID-19 should make us step up our game when it comes to mental health treatments in general, and “that should include psychedelics as well, because they are so promising.”
While opinions vary on whether a predicted increase in PTSD necessitates accelerating psychedelics research, it’s clear that such studies need to continue in the same evidence-based fashion they have been, and that easing legal restrictions and dismantling the stigma around them would help — for all those living with this painful disorder, whether it arose as a result of the pandemic, or not.